Cystic
Fibrosis
part-2
Return
to
page-1
Gut symptoms
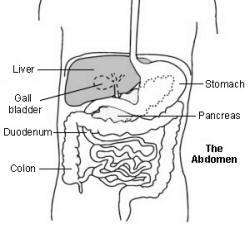
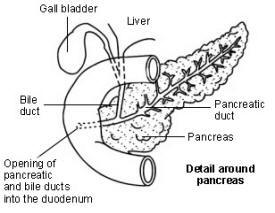
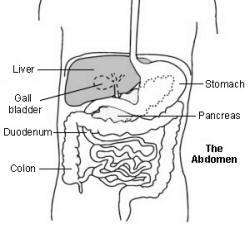
The pancreas normally makes
digestive juices which contain
chemicals (enzymes). The digestive
juices normally flow out from the
pancreatic duct into the duodenum
and digest food.
In people with cystic fibrosis,
thickened secretions block the
normal flow of the digestive juices
from the pancreas. This can result
in food not being digested or
absorbed properly, in particular,
fatty foods and fat-soluble vitamins
(vitamins A, D, E and K). This can
cause:
- Malnutrition leading to poor
growth and poor weight gain
(even if you have a good
appetite and eat a lot, as the
problem is with digesting and
absorbing the food).
- Large, smelly, greasy, fatty
faeces (stools or motions) occur
in about a third of cases.
- Bloated abdomen.
In about 3 in 20 cases the
pancreas functions well and there
are no or minimal gut symptoms, and
mainly just lung symptoms.
Symptoms sometimes occur at
birth
About 1 in 10 children with cystic
fibrosis are diagnosed shortly after
birth. This is due to a condition
called meconium ileus where in some
cases the gut becomes blocked with
meconium - a thick, dark, sticky
substance which is made by the
baby's gut before being born. Urgent
surgery may be needed to relieve the
blockage.
Other symptoms and
complications
Other organs may be affected which
may cause various other problems in
some cases. Also, the pancreas and
airways may become severely
affected. Therefore, other problems
which may also occur in some cases
include:
- Repeated sinus infections.
- Polyps forming in the nose.
- Infertility (especially in
males as the tubes which carry
the sperm can become blocked).
- Damage to the liver which
may lead to cirrhosis occurs in
about 1 in 12 cases (if the
small ducts in the liver become
blocked or damaged).
- Diabetes. (Special cells in
the pancreas make insulin. If
the pancreas becomes severely
damaged over time then insulin
levels go down and diabetes may
develop.) This is rare in
children but is more common in
adults who have had cystic
fibrosis for years.
- Pancreatitis (inflammation
of the pancreas).
- Rectal prolapse.
- Constipation.
- Osteoporosis (thinning of
the bones) may develop due to
poor absorption of food, and in
particular, poor absorption of
vitamin D which is needed to
maintain healthy bones.
- The sweat tastes very salty.
General
Ongoing poor nutrition combined with
persistent lung symptoms and
repeated chest infections often
causes 'failure to thrive' in young
children, delayed maturation and
sexual development in teenagers, and
general poor health at any age.
Mild cases
Recently, some cases of cystic
fibrosis have been diagnosed in
adults who have relatively mild
symptoms. This may be due to some
mutations of the cystic fibrosis
gene not being as 'faulty' as
others. The handling of sodium and
chloride may only be mildly affected
in these cases.
How is cystic fibrosis
diagnosed?
Sweat test
A doctor may arrange a sweat test if
he or she suspects cystic fibrosis
from the symptoms. This test
measures the amount of salt (sodium
and chloride) in skin sweat. People
with cystic fibrosis have an
abnormally high salt level in sweat.
Genetic test
A genetic test can confirm the
diagnosis. Some cells are scrapped
from the inside of the cheek. These
can be tested to detect the cystic
fibrosis gene.
Screening test
Some countries screen all newborn
babies for cystic fibrosis. A small
'heel prick' blood test is taken
about the sixth day after birth.
This can detect a chemical called
immunoreactive trypsin which is high
in babies with cystic fibrosis. If
it is high then a sweat test and
genetic test can be done to confirm
the diagnosis.
There are very good arguments to
screen all babies as the earlier the
diagnosis is made, the sooner
treatment can begin which improves
the outlook (prognosis). However,
only a few places in the UK
routinely screen newborn babies for
cystic fibrosis. This may change in
the future and screening may be
introduced to include all areas in
the UK.
What is the treatment for
cystic fibrosis?
There are many aspects to the
treatment of people with cystic
fibrosis. Treatment involves the
input, advice, and expertise of
various professionals such as child
health doctors, specialist nurses,
physiotherapists, dieticians, etc.
It is usual to have regular checks
and tests to monitor the condition
and to keep a check on children's
growth, development and well-being.
The following list is a brief
overview of the commonly used
treatments, but is not a full or
exhaustive account of all the
treatments used. An individual
treatment plan is needed for each
case to take into account individual
circumstances.
All patients need to on
celiac diet.
All patients should use a
electronic zapper, or Tens unit
everyday.
Treatments for lung problems
Physiotherapy and exercise
Regular chest physiotherapy is very
important. This helps to clear the
airways of the thick mucus. A
physiotherapist usually shows
parents how to do this for their
children. It involves a special way
to firmly pat the chest whilst the
child lies head-down to encourage
mucus and sputum to be coughed out.
Twice daily chest physiotherapy is
common practice. This may need to be
increased during times of chest
infections. It is also important to
encourage children to exercise and
to be as active and fit as possible.
So, sports and games are encouraged.
Antibiotics and antifungals
Courses of antibiotics are a
mainstay of treatment specially
doxycycline. Many children with
cystic fibrosis take regular
long-term antibiotics. The dose is
increased and/or other types of
antibiotics are given when a chest
infection develops. Various bacteria
can cause infections and the
antibiotics chosen depend on which
bacteria are found in samples of
sputum. Antibiotics given
intravenously (into a vein) are
often required for severe infections
that are not controlled with
antibiotic tablets.
A bacterium called pseudomonas
aeruginosa commonly persists in
the thick mucus in the airways. To
keep this from flaring up into
repeated infections, an antibiotic
given by nebuliser (inhaled
antibiotic) is a common treatment.
Further help and
information
Return back to first
page of Cystic Fibrosis
Internet help Available
see our services & contact information
The pancreas normally makes digestive juices which contain chemicals (enzymes). The digestive juices normally flow out from the pancreatic duct into the duodenum and digest food.
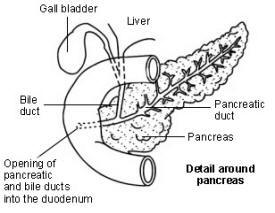
In people with cystic fibrosis, thickened secretions block the normal flow of the digestive juices from the pancreas. This can result in food not being digested or absorbed properly, in particular, fatty foods and fat-soluble vitamins (vitamins A, D, E and K). This can cause:
- Malnutrition leading to poor growth and poor weight gain (even if you have a good appetite and eat a lot, as the problem is with digesting and absorbing the food).
- Large, smelly, greasy, fatty faeces (stools or motions) occur in about a third of cases.
- Bloated abdomen.
In about 3 in 20 cases the pancreas functions well and there are no or minimal gut symptoms, and mainly just lung symptoms.
Symptoms sometimes occur at
birth
About 1 in 10 children with cystic
fibrosis are diagnosed shortly after
birth. This is due to a condition
called meconium ileus where in some
cases the gut becomes blocked with
meconium - a thick, dark, sticky
substance which is made by the
baby's gut before being born. Urgent
surgery may be needed to relieve the
blockage.
Other symptoms and
complications
Other organs may be affected which
may cause various other problems in
some cases. Also, the pancreas and
airways may become severely
affected. Therefore, other problems
which may also occur in some cases
include:
- Repeated sinus infections.
- Polyps forming in the nose.
- Infertility (especially in males as the tubes which carry the sperm can become blocked).
- Damage to the liver which may lead to cirrhosis occurs in about 1 in 12 cases (if the small ducts in the liver become blocked or damaged).
- Diabetes. (Special cells in the pancreas make insulin. If the pancreas becomes severely damaged over time then insulin levels go down and diabetes may develop.) This is rare in children but is more common in adults who have had cystic fibrosis for years.
- Pancreatitis (inflammation of the pancreas).
- Rectal prolapse.
- Constipation.
- Osteoporosis (thinning of the bones) may develop due to poor absorption of food, and in particular, poor absorption of vitamin D which is needed to maintain healthy bones.
- The sweat tastes very salty.
General
Ongoing poor nutrition combined with
persistent lung symptoms and
repeated chest infections often
causes 'failure to thrive' in young
children, delayed maturation and
sexual development in teenagers, and
general poor health at any age.
Mild cases
Recently, some cases of cystic
fibrosis have been diagnosed in
adults who have relatively mild
symptoms. This may be due to some
mutations of the cystic fibrosis
gene not being as 'faulty' as
others. The handling of sodium and
chloride may only be mildly affected
in these cases.
How is cystic fibrosis diagnosed?
Sweat test
A doctor may arrange a sweat test if
he or she suspects cystic fibrosis
from the symptoms. This test
measures the amount of salt (sodium
and chloride) in skin sweat. People
with cystic fibrosis have an
abnormally high salt level in sweat.
Genetic test
A genetic test can confirm the
diagnosis. Some cells are scrapped
from the inside of the cheek. These
can be tested to detect the cystic
fibrosis gene.
Screening test
Some countries screen all newborn
babies for cystic fibrosis. A small
'heel prick' blood test is taken
about the sixth day after birth.
This can detect a chemical called
immunoreactive trypsin which is high
in babies with cystic fibrosis. If
it is high then a sweat test and
genetic test can be done to confirm
the diagnosis.
There are very good arguments to screen all babies as the earlier the diagnosis is made, the sooner treatment can begin which improves the outlook (prognosis). However, only a few places in the UK routinely screen newborn babies for cystic fibrosis. This may change in the future and screening may be introduced to include all areas in the UK.
What is the treatment for cystic fibrosis?
There are many aspects to the treatment of people with cystic fibrosis. Treatment involves the input, advice, and expertise of various professionals such as child health doctors, specialist nurses, physiotherapists, dieticians, etc. It is usual to have regular checks and tests to monitor the condition and to keep a check on children's growth, development and well-being.
The following list is a brief overview of the commonly used treatments, but is not a full or exhaustive account of all the treatments used. An individual treatment plan is needed for each case to take into account individual circumstances.
All patients need to on celiac diet.
All patients should use a electronic zapper, or Tens unit everyday.
Treatments for lung problems
Physiotherapy and exercise
Regular chest physiotherapy is very
important. This helps to clear the
airways of the thick mucus. A
physiotherapist usually shows
parents how to do this for their
children. It involves a special way
to firmly pat the chest whilst the
child lies head-down to encourage
mucus and sputum to be coughed out.
Twice daily chest physiotherapy is
common practice. This may need to be
increased during times of chest
infections. It is also important to
encourage children to exercise and
to be as active and fit as possible.
So, sports and games are encouraged.
Antibiotics and antifungals
Courses of antibiotics are a
mainstay of treatment specially
doxycycline. Many children with
cystic fibrosis take regular
long-term antibiotics. The dose is
increased and/or other types of
antibiotics are given when a chest
infection develops. Various bacteria
can cause infections and the
antibiotics chosen depend on which
bacteria are found in samples of
sputum. Antibiotics given
intravenously (into a vein) are
often required for severe infections
that are not controlled with
antibiotic tablets.
A bacterium called pseudomonas aeruginosa commonly persists in the thick mucus in the airways. To keep this from flaring up into repeated infections, an antibiotic given by nebuliser (inhaled antibiotic) is a common treatment.
Further help and information
Return back to first page of Cystic Fibrosis
Internet help Available see our services & contact information