;Acute Kidney Failure & information Welcome to cidpusa.org | |||
| Guide to natural treatment of diseases Flame within book. | |||
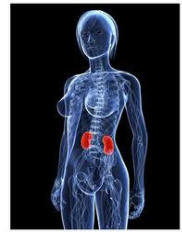
| Definition Acute kidney failure occurs when illness, infection, or injury damages the kidneys. Temporarily, the kidneys cannot adequately remove fluids and wastes from the body or maintain the proper level of certain kidney-regulated chemicals in the bloodstream.
Return to page one Treatment Treatment for acute kidney failure varies. Treatment is directed to the underlying, primary medical condition that has triggered kidney failure. Prerenal conditions may be treated with replacement fluids given through a vein, diuretics, blood transfusion, or medications. Postrenal conditions and intrarenal conditions may require surgery and/or medication. Frequently, patients in acute kidney failure require hemodialysis, hemofiltration, or peritoneal dialysis to filter fluids and wastes from the bloodstream until the primary medical condition can be controlled. Hemodialysis Hemodialysis involves circulating the patient's blood outside of the body through an extracorporeal circuit (ECC), or dialysis circuit. The ECC is made up of plastic blood tubing, a filter known as a dialyzer (or artificial kidney), and a dialysis machine that monitors and maintains blood flow and administers dialysate. Dialysate is a sterile chemical solution that is used to draw waste products out of the blood. The patient's blood leaves the body through the vein and travels through the ECC and the dialyzer, where fluid removal takes place. During dialysis, waste products in the bloodstream are carried out of the body. At the same time, electrolytes and other chemicals are added to the blood. The purified, chemically-balanced blood is then returned to the body. A dialysis "run" typically lasts three to four hours, depending on the type of dialyzer used and the physical condition of the patient. Dialysis is used several times a week until acute kidney failure is reversed. Blood pressure changes associated with hemodialysis may pose a risk for patients with heart problems. Peritoneal dialysis may be the preferred treatment option in these cases. Hemofiltration Hemofiltration, also called continuous renal replacement therapy (CRRT), is a slow, continuous blood filtration therapy used to control acute kidney failure in critically ill patients. These patients are typically very sick and may have heart problems or circulatory problems. They cannot handle the rapid filtration rates of hemodialysis. They also frequently need antibiotics, nutrition, vasopressors, and other fluids given through a vein to treat their primary condition. Because hemofiltration is continuous, prescription fluids can be given to patients in kidney failure without the risk of fluid overload. Like hemodialysis, hemofiltration uses an ECC. A hollow fiber hemofilter is used instead of a dialyzer to remove fluids and toxins. Instead of a dialysis machine, a blood pump makes the blood flow through the ECC. The volume of blood circulating through the ECC in hemofiltration is less than that in hemodialysis. Filtration rates are slower and gentler on the circulatory system. Hemofiltration treatment will generally be used until kidney failure is reversed. Peritoneal dialysis Peritoneal dialysis may be used if an acute kidney failure patient is stable and not in immediate crisis. In peritoneal dialysis (PD), the lining of the patient's abdomen, the peritoneum, acts as a blood filter. A flexible tube-like instrument (catheter) is surgically inserted into the patient's abdomen. During treatment, the catheter is used to fill the abdominal cavity with dialysate. Waste products and excess fluids move from the patient's bloodstream into the dialysate solution. After a certain time period, the waste-filled dialysate is drained from the abdomen, and replaced with clean dialysate. There are three type of peritoneal dialysis, which vary according to treatment time and administration method. Peritoneal dialysis is often the best treatment option for infants and children. Their small size can make vein access difficult to maintain. It is not recommended for patients with abdominal adhesions or other abdominal defects (like a hernia) that might reduce the efficiency of the treatment. It is also not recommended for patients who suffer frequent bouts of an inflammation of the small pouches in the intestinal tract (diverticulitis). Prognosis Because many of the illnesses and underlying conditions that often trigger acute kidney failure are critical, the prognosis for these patients many times is not good. Studies have estimated overall death rates for acute kidney failure at 42-88%. Many people, however, die because of the primary disease that has caused the kidney failure. These figures may also be misleading because patients who experience kidney failure as a result of less serious illnesses (like kidney stones or dehydration) have an excellent chance of complete recovery. Early recognition and prompt, appropriate treatment are key to patient recovery. Up to 10% of patients who experience acute kidney failure will suffer irreversible kidney damage. They will eventually go on to develop chronic kidney failure or end-stage renal disease. These patients will require long-term dialysis or kidney transplantation to replace their lost renal functioning. Prevention Since acute kidney failure can be caused by many things, prevention is possiable. Medications that may impair kidney function should be given cautiously. Patients with pre-existing kidney conditions who are hospitalized for other illnesses or injuries should be carefully monitored for kidney failure complications. Treatments and procedures that may put them at risk for kidney failure (like diagnostic tests requiring radiocontrast agents or dyes) which include MRI, CAT SCAN should be used with extreme caution. Treat throat infections promptly, do take omega-3 daily to reduce inflammation. Clean teeth with hydrogen peroxide to prevent dental disease and follow the instructions on the diet page of cidpusa.org link is on the top of this page. Key Terms
Acute kidney failure occurs when illness, infection, or injury damages the kidneys | |||