Acute renal failure in patients with congestive heart failure occurs because of decreased renal blood flow. This decrease is due to hypovolemia from overdiuresis or hypervolemia that causes elevated filling pressures of the left ventricle and leads to decreased cardiac output. Patients in the former group may respond to the discontinuation of diuretics and gentle hydration. Patients in the latter group are treated with diuretics and may need inotropes and vasodilators. Invasive hemodynamic monitoring may be required for fluid management.
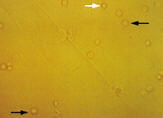
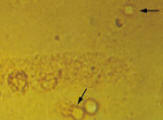
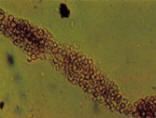
Intrinsic Acute Renal Failure Intrinsic acute renal failure is subdivided into four categories: tubular disease, glomerular disease, vascular disease and interstitial disease. In intrinsic acute renal failure, the renal parenchyma is injured. The damage to tubule cells leads to certain urine microscopic findings (Table 63 and Figures 2 and 3). Parenchymal injury causes impaired sodium reabsorption and results in a fractional excretion of sodium of greater than 3 percent and an isotonic urine osmolality of 250 to 300 mOsm (Table 7).
Tubular Disease In ischemic acute tubular necrosis, unlike prerenal acute renal failure, the glomerular filtration rate does not improve with the restoration of renal blood flow. Ischemic acute tubular necrosis is frequently reversible, but if the ischemia is severe enough to cause cortical necrosis, irreversible renal failure can occur.2,3 Contrast agents and aminoglycosides are the agents most often associated with acute tubular necrosis. The condition can also be caused by pigment from myoglobinuria (rhabdomyolysis) or hemoglobinuria (hemolysis).
Acute tubular necrosis has three phases.2 Renal injury evolves during the initiation phase, which lasts hours to days. In the maintenance phase, which lasts days to weeks, the glomerular filtration rate reaches its nadir and urine output is at its lowest. The recovery phase lasts days, often beginning with postacute tubular necrosis diuresis. Hypovolemia from excess urine output is a concern during this phase. Despite recovery of urine production, patients can still have difficulty with uremia and homeostasis of electrolytes and acid because tubular function is not completely recovered. Diligent monitoring is indicated throughout all phases of acute tubular necrosis.
|