Myopericarditis following smallpox vaccination among vaccinia-naive US military personnel.
The University of Virginia, Charlottesville, USA.
In the United States, the annual incidence of myocarditis is estimated at 1 to 10 per 100,000 population.
As many as 1% to 5% of patients with acute viral infections involve the myocardium. Although many viruses have been reported to cause myopericarditis.
A rare or unrecognized event after vaccination with the currently used strain of vaccinia virus has caused Myocarditis after a simple vaccine.(New York City Board of Health).
OBJECTIVE: To describe a series of probable cases of myopericarditis following smallpox vaccination among US military service members reported since the reintroduction of vaccinia vaccine.
DESIGN, SETTING, PARTICIPANTS: Surveillance case definitions are presented. The cases were identified either through sentinel reporting to US military headquarters surveillance using the Defense Medical Surveillance System or reports to the Vaccine Adverse Event Reporting System using International Classification of Diseases, Ninth Revision. The cases occurred among individuals vaccinated from mid-December 2002 to March 14, 2003.
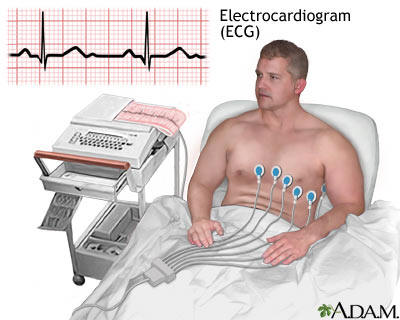
MAIN OUTCOME MEASURE: Elevated serum levels of creatine kinase (MB isoenzyme), troponin I, and troponin T, usually in the presence of ST-segment elevation on electrocardiogram and wall motion abnormalities on echocardiogram.
RESULTS: Among 230,734 primary vaccinees, 18 cases of probable myopericarditis after smallpox vaccination were reported (an incidence of 7.8 per 100,000 over 30 days). No cases of myopericarditis following smallpox vaccination were reported among 95,622 vaccinees who were previously vaccinated.
All cases were white men aged 21 years to 33 years (mean age, 26.5 years), who presented with acute myopericarditis 7 to 19 days following vaccination. A causal relationship is supported by the close temporal clustering (7-19 days; mean, 10.5 days following vaccination), wide geographic and temporal distribution, occurrence in only primary vaccinees, and lack of evidence for alternative etiologies or other diseases associated with myopericarditis. Additional supporting evidence is the observation that the observed rate of myopericarditis among primary vaccinees is 3.6-fold (95% confidence interval, 3.33-4.11) higher than the expected rate among personnel who were not vaccinated. The background incidence of myopericarditis did not show statistical significance when stratified by age (20-34 years: 2.18 expected cases per 100,000; 95% confidence interval [CI], 1.90-2.34), race (whites: 1.82 per 100,000; 95% CI, 1.50-2.01), and sex (males: 2.28 per 100,000; 95% CI, 2.04-2.54).
CONCLUSION: Among US military personnel vaccinated against smallpox, myopericarditis occurred at a rate of 1 per 12 819 primary vaccinees. Myopericarditis should be considered an expected adverse event associated with smallpox vaccination. Clinicians should consider myopericarditis in the differential diagnosis of patients presenting with chest pain 4 to 30 days following smallpox vaccination and be aware of the implications as well as the need to report this potential adverse advent.